By Lynda Williams, medwireNews Reporter
medwireNews: Danish researchers have quantified the risk of second primary malignancy (SPM) in patients with lymphoma who are treated with high-dose chemotherapy and autologous haematopoietic stem-cell transplantation (HSCT).
Adults who underwent this treatment regimen between 2001 and 2017 were a significant 2.35 times more likely than matched controls from the general population to experience an SPM over a median 7.76 years of follow-up, report Trine Trab (Rigshospitalet, Copenhagen) and colleagues in The Lancet Haematology.
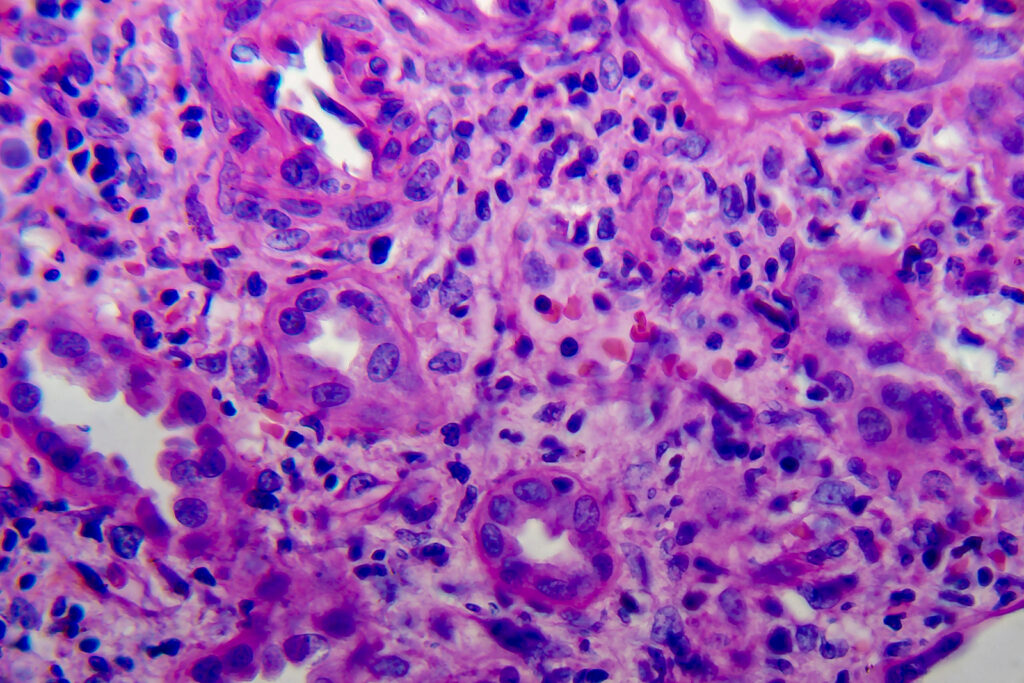
This included a significantly greater risk of non-melanoma skin cancer (hazard ratio [HR]=2.94) and myelodysplastic syndrome or acute myeloid leukaemia (AML; HR=41.13), after adjusting for a raft of confounding factors including age, sex, education and comorbidity.
By contrast, receipt of high-dose chemotherapy and autologous HSCT did not significantly increase the risk of a solid SPM compared with the general population, the team says.
“Our findings are of clinical importance when comparing the risks and benefits for patients with lymphoma who are being considered for high-dose chemotherapy and autologous HSCT, and for making the best-informed treatment decisions when alternative treatment options are available”, Trab et al write.
The authors of an accompanying comment agree, emphasizing that the risk of SPM after autologous HSCT “must be visualised in the context of other newly developed and potentially curative treatment strategies in patients with lymphomas”, such as the use of CAR T-cell therapy.
“The specificity of the therapy reduces damage to healthy cells that are associated with conventional treatments and, despite little data regarding the development of SPMs due to the small number of patients who have been treated and short follow-up, development of SPMs does not appear to be a substantial side-effect with this therapeutic strategy”, observe Anna Sureda and Eva Domingo-Domenech, from the Universitat de Barcelona in Spain.
They suggest that the current analysis “highlights the importance of analysing pre-transplantation clonal haematopoiesis and assessing the risk-benefit ratio of this strategy compared with other therapeutic options.”
The population-based cohort study included 803 patients with aggressive diffuse large B-cell lymphoma (DLBCL), mantle cell lymphoma, Hodgkin lymphoma or nodal peripheral T-cell lymphoma (67% men; median age 57 years) and 4015 controls matched by birth year and sex.
The majority of patients were treated with high-dose chemotherapy and autologous HSCT at first relapse but almost a third of the DLBCL cohort were given this as a first-line approach, the study authors say.
After adjustment, the 5-, 10- and 15-year cumulative risk of first SPM among patients given high-dose chemotherapy and autologous HSCT was 12%, 20% and 24%, respectively. The corresponding cumulative risks for the controls were 7%, 14% and 21%.
Five-year survival was achieved by 67% of patients and 96% of controls.
Of note, older patients who received high-dose chemotherapy and autologous HSCT were significantly more likely to develop an SPM than younger patients (HR=1.06 per year) as were those with than without an alcohol-related disease (HR=3.11). And men receiving the treatment appeared to be more likely than their female counterparts to develop a non-melanoma skin cancer or myelodysplastic syndrome/AML.
News stories are provided by medwireNews, which is an independent medical news service provided by Springer Healthcare Ltd. © 2023 Springer Healthcare Ltd, part of the Springer Nature Group
Lancet Haematol 2023; 10.1016/S2352-3026(23)00212-0
https://pubmed.ncbi.nlm.nih.gov/37689081/
Lancet Haematol 2023; 10.1016/S2352-3026(23)00248-X