By Lynda Williams, medwireNews Reporter
medwireNews: Phase 1–2 trial findings indicate that the cereblon E3 ubiquitin ligase modulator mezigdomide, given in combination with dexamethasone, could offer a novel oral regimen for patients with heavily pretreated multiple myeloma.
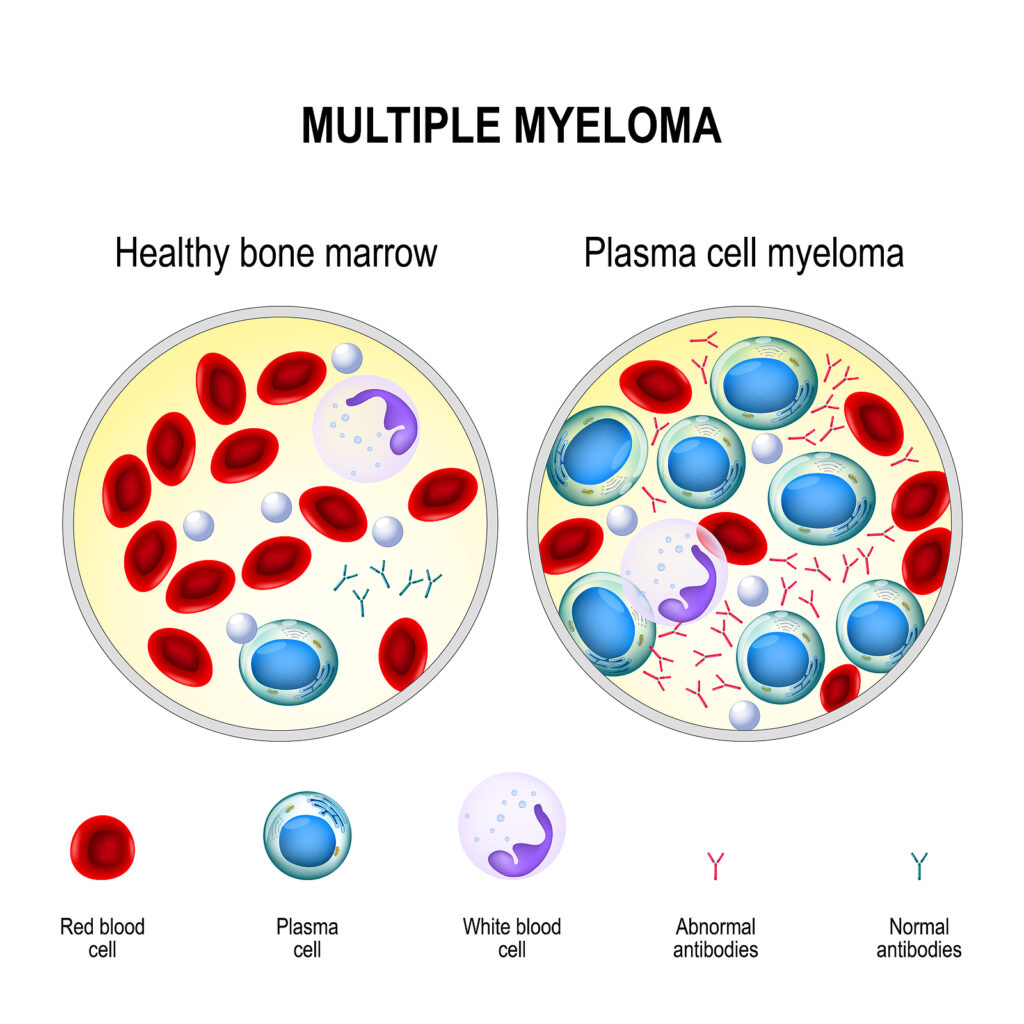
“Mezigdomide was specifically designed to achieve rapid, potent, and deep degradation of Ikaros and Aiolos, key transcription factors in hematopoietic cell development and differentiation”, explain Paul Richardson (Dana-Farber Cancer Institute, Boston, Massachusetts, USA) and fellow CC-92480-MM-001 investigators.
They report in The New England Journal of Medicine that there was “promising preliminary efficacy” even among patients with disease refractory to lenalidomide and pomalidomide, and that the “acceptable” safety profile means “dosing options for mezigdomide plus dexamethasone in combination with other agents will continue to be explored.”
Overall, 77 patients were enrolled in phase 1, all of whom had previously received at least three lines of therapy including lenalidomide, pomalidomide, a proteasome inhibitor, a glucocorticoid and an anti-CD38 antibody.
Multiple continuous and intermittent-intensive dosing schedules were trialed in parallel and the maximum tolerated dose of 1.0 mg/day plus dexamethasone on 21 days of each 28-day cycle was selected as the phase 2 recommended regimen.
The most common grade 3 and 4 adverse events (AEs) in the dose-escalation cohort were neutropenia (23% and 48%, respectively), infection (36% and 4%) and anaemia (38% and 0%) and there was one treatment-related death from brain abscess. An overall response was reported for 25% of the enrolled patients, rising to 55% among the 11 patients given the recommended phase 2 schedule.
For phase 2, 101 patients with triple-class-refractory multiple myeloma were recruited. The patients had received a median six lines of prior therapy, including stem cell transplantation in 77% and anti-B-cell maturation antigen (anti-BCMA) therapy in 30%, while 40% of patients had plasmacytomas.
After a median four cycles of therapy, the most common grade 3 or 4 AEs were neutropenia (22% and 54%, respectively), infection (29% and 6%), anaemia (35% and 1%) and febrile neutropenia (13% and 2%).
AEs led to mezigdomide dose reductions in 29% of patients and discontinuation in 6%, and 77% of patients required granulocyte colony-stimulating factor to treat neutropenia or as prophylaxis against neutropenia.
After a median follow-up of 7.5 months, the overall response rate was 41%, including a stringent complete response in 2%, a complete response in 3%, a very good partial response in 20% and a partial response in 16%. The median duration of response was 7.6 months at the time of reporting and the median progression-free survival was 4.4 months, with follow-up for overall survival continuing.
Responses were noted in 30% of patients with plasmacytomas and 50% of those with prior anti-BCMA therapy, as well as in 32% of participants with high-risk cytogenetic abnormalities, such as 17p deletion or 1q21 amplification.
Richardson and co-investigators also note that “robust increases in proliferating (Ki-67+) T cells and an immunophenotypic shift toward an activated or effector memory phenotype” occurred among the patients given the recommended phase 2 schedule.
Given this response was found among participants whose most recent treatment had been pomalidomide, the authors suggest that “mezigdomide remains immune-stimulatory” after this therapy.
News stories are provided by medwireNews, which is an independent medical news service provided by Springer Healthcare Ltd. © 2023 Springer Healthcare Ltd, part of the Springer Nature Group
New Engl J Med 2023; doi:10.1056/NEJMoa2303194