By Laura Cowen, medwireNews Reporter
medwireNews: Apixaban does not significantly reduce the rate of venous thromboembolism (VTE) relative to standard care in paediatric patients with acute lymphoblastic leukaemia (ALL) or lymphoma, show data from the phase 3 PREVAPIX-ALL trial.
Based on these findings, “apixaban cannot be recommended for routine thromboprophylaxis” in such patients, write Sarah O’Brien (The Ohio State University, Columbus, USA) and co-authors in The Lancet Haematology.
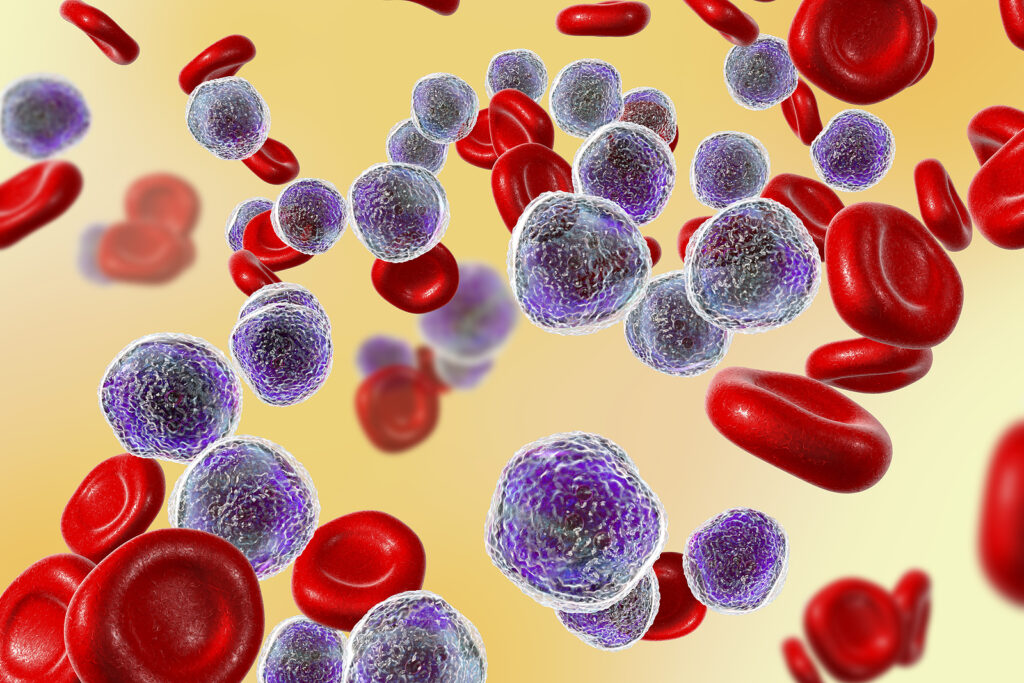
They explain: “Paediatric patients with acute lymphoblastic leukaemia or lymphoma are at increased risk of venous thromboembolism resulting in increased mortality and morbidity.”
The previously published THROMBOTECT study showed that low molecular weight heparin significantly lowered VTE risk in this setting, but the acceptability of the treatment, which is given via daily subcutaneous injection, “was a substantial issue”, O’Brien et al remark.
To address this, they randomly assigned 512 participants (57% male) aged 1 year to 17 years with newly diagnosed ALL (pre-B cell or T cell) or lymphoblastic lymphoma (B cell or T cell immunophenotype) to receive weight-adjusted twice-daily treatment with the oral direct Factor Xa inhibitor apixaban during induction (n=256) or standard care (ie, no systemic anticoagulation; n=256).
During a median 27 days of follow-up, 12% of patients in the apixaban arm were diagnosed with a symptomatic VTE or a clinically unsuspected VTE detected by ultrasound and echocardiogram at the end of induction. By comparison, the rate was 18% among the participants in the standard care arm, a nonsignificant difference. The researchers suggest that the lack of statistical significance could be a result of the short follow-up period and limited exposure to apixaban.
There were two major bleeding events in each arm, but the rate of clinically relevant nonmajor (CRNM) bleeding, primarily grade 1 or 2 epistaxis, was significantly higher with apixaban than with standard care, at 4% versus 1%.
Of note, a post-hoc analysis showed that the impact of apixaban on bleeding events differed by age. In participants younger than 10 years (n=179 per group), major or CRNM bleeding occurred in 4% of participants receiving apixaban compared with 1% of those receiving standard care. For participants aged 10 years and older (n=77 per group), the rates were similar between the study groups, at 6% versus 5%.
The researchers conclude that although “apixaban cannot be recommended for routine thromboprophylaxis”, its “safety profile, paediatric formulation, and ease of administration” mean that it “could be considered when thromboprophylaxis is desired for paediatric patients with acute lymphoblastic leukaemia or lymphoma who have an increased risk of venous thromboembolism.”
In an accompanying comment, Uma Athale, from McMaster University in Hamilton, Ontario, Canada, points out that the majority (86%) of the total thromboembolism events were asymptomatic. She therefore questions whether “patients and physicians [are] willing to accept the added risk of bleeding to prevent an asymptomatic clot when the clinical significance of the clot is unknown or is associated with a remote possibility of post-thrombotic syndrome.”
Athalesays that “future thromboprophylaxis trial designs need to carefully select the study population and aim to prevent clinically significant adverse outcomes.”
News stories are provided by medwireNews, which is an independent medical news service provided by Springer Healthcare Ltd. © 2024 Springer Healthcare Ltd, part of the Springer Nature Group
Lancet Haematol 2023; doi:10.1016/S2352-3026(23)00314-9
https://pubmed.ncbi.nlm.nih.gov/37980924/
Lancet Haematol 2023; doi:10.1016/S2352-3026(23)00339-3
https://pubmed.ncbi.nlm.nih.gov/37980925/